"I've been driving since before you were born! I know how to drive!"
This familiar phrase often marks the beginning of a difficult conversation between older adults and their families about driving. For many older adults, driving is more than just a means of getting around; it's a key part of their independence and identity. However, as we age, physical and cognitive changes can make driving more challenging and potentially dangerous. Understanding when it’s time to stop driving is crucial, not only for the safety of the driver but also for everyone on the road. This guide explores the signs that it might be time to reconsider driving, strategies for assessing driving abilities, ways to have sensitive conversations, and resources to support a smooth transition to alternative transportation.
Recognizing the Signs: When to Reevaluate Driving Abilities
Aging can lead to various changes that may impact driving safety:
Physical Declines: Vision loss, hearing impairment, arthritis, and slower reaction times can significantly impact an older adult's driving ability. Reduced peripheral vision or difficulty judging distances can lead to unsafe situations, especially in busy or complex traffic conditions.
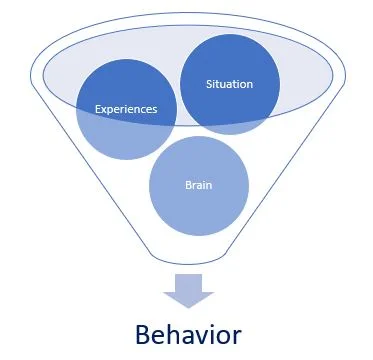
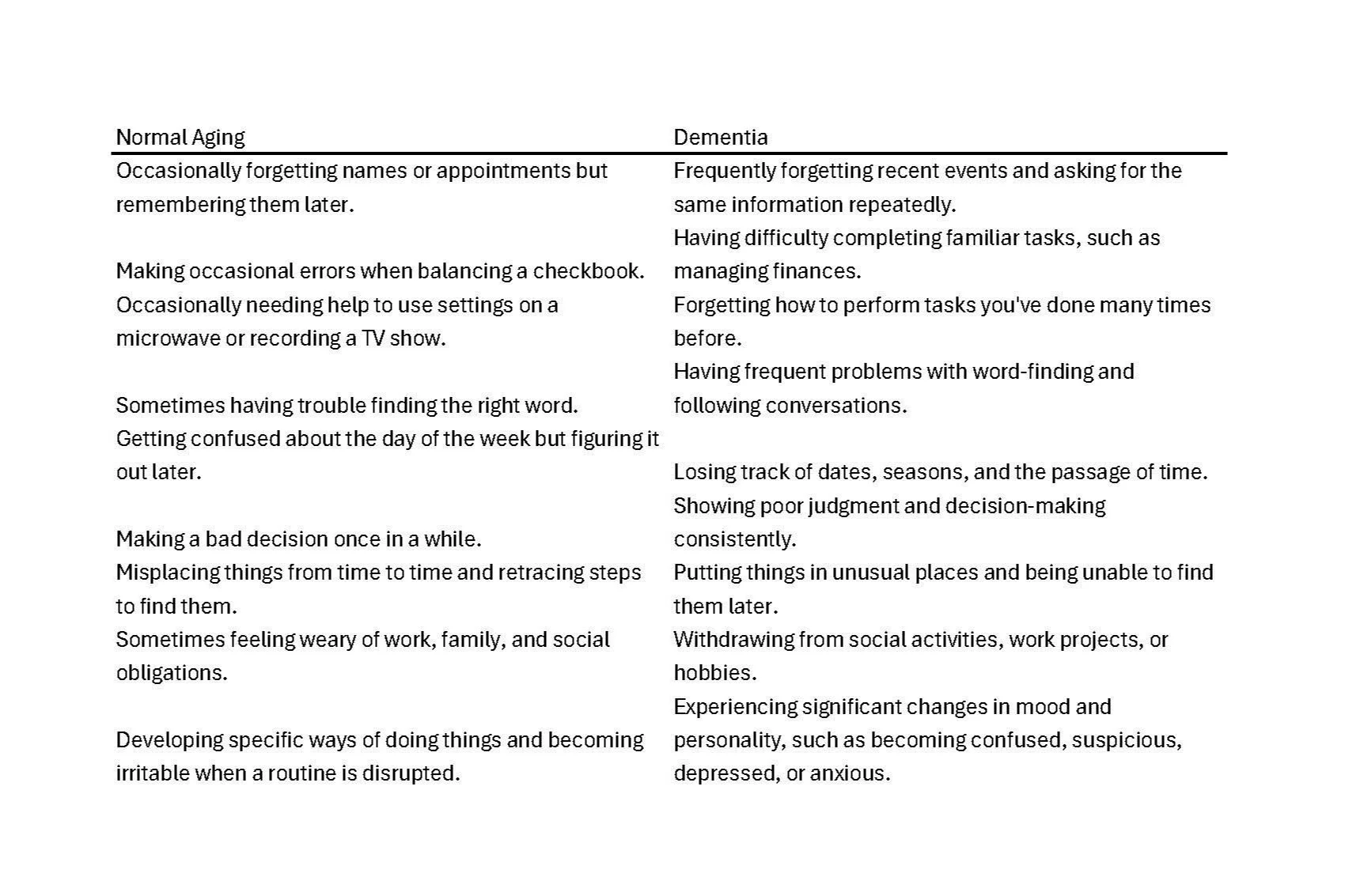
Cognitive Declines: Cognitive impairments such as slowed processing speed, poor executive functioning, visuospatial deficits, and significant memory loss are common in older adults and can severely impact driving skills. These issues can cause delays in reaction times, difficulties in navigating, or an increased likelihood of getting lost, even in familiar areas. Such cognitive changes can also affect decision-making abilities, making it harder to respond appropriately in fast-changing traffic situations(WashU Med,PubMed).
Behavioral Changes: Specific signs that an older adult's driving might be declining include getting lost on familiar routes, drifting between lanes, frequent minor accidents, or an increased hesitance to drive at night or on highways.
Strategies for Assessing Driving Abilities
Drive-Along Evaluations: One practical approach for families is to spend time driving with their loved one as a passenger. This allows them to observe their driving skills firsthand. Pay attention to key indicators such as difficulty in maintaining lane position, delayed reactions to traffic signals, and confusion in navigating known routes. If family members feel too afraid to ride along with their loved one, this itself is a significant warning sign that should not be ignored.
Professional Driving Evaluations: Another valuable yet often underutilized resource is a professional driving evaluation. These evaluations can be conducted through hospital rehabilitation programs or specialized driving schools. They provide an objective assessment of an individual’s driving skills and offer recommendations on whether it is safe for the person to continue driving. Occupational therapists who specialize in driver rehabilitation can assess both physical and cognitive abilities, provide adaptive equipment, or suggest strategies to compensate for any deficits. These evaluations can also help tailor training programs to address specific challenges faced by older drivers.
How to Approach the Conversation: Tips for Families
Discussing driving cessation with an older adult is never easy, but it is essential for their safety and the safety of others on the road. Here are some strategies to guide the conversation:
Start the Conversation Early: Don’t wait for an accident or a close call to have the discussion. Bringing up the topic early allows for more time to assess abilities, explore options, and emotionally prepare for the transition.
Use Empathy and Respect: Understand that driving is a sensitive subject tied to an individual’s sense of independence. Approach the topic with empathy and focus on your concern for their safety and the safety of others.
Present Objective Evidence: Use specific examples of unsafe driving behaviors or results from recent cognitive assessments to illustrate concerns. If professional driving evaluations have been conducted, share those results to provide an objective basis for the discussion.
Involve Healthcare Professionals: Bringing in a third party, such as a doctor or an occupational therapist, can help provide an unbiased perspective. Healthcare professionals can help explain the risks and provide recommendations for next steps.
Transitioning from Driving: Maintaining Independence
Stopping driving doesn’t mean giving up independence. Here are some strategies to help maintain quality of life:
Explore Transportation Alternatives: Look into public transit, rideshare services, community shuttles, and volunteer driver programs. Many communities offer resources specifically designed to assist older adults.
Encourage Social Engagement: Encourage participation in activities that don’t require driving, such as joining local clubs, attending senior center activities, or participating in community events. Staying socially active can help prevent isolation, a common concern when someone stops driving.
Provide Practical Support: Family members and friends can offer rides and check in regularly, ensuring the older adult remains socially active and engaged.
Conclusion: Balancing Safety and Independence
Deciding when to stop driving is a deeply personal and often emotional decision. By recognizing the signs of declining driving ability, understanding the impact of cognitive changes, and approaching the conversation with empathy and respect, families can help their loved ones transition safely while preserving their independence as much as possible. Early planning and considering all factors—from health and safety to emotional well-being—will help make the best decision for everyone involved. Utilizing resources like drive-along evaluations and professional driving assessments can provide valuable insights and support in making this important decision.
FAQ: Common Questions About Older Adults and Driving
1. Can a doctor take away an older adult's driver's license?
A doctor cannot directly revoke an older adult’s driver's license. However, they can recommend that a patient stops driving if they believe it is unsafe due to physical or cognitive impairments. In some cases, doctors are mandated by law to report patients with certain medical conditions to the Department of Motor Vehicles (DMV), who then has the authority to evaluate the individual's ability to drive and possibly revoke or restrict their license.
2. What should families do if an older adult is resistant to stopping driving?
Resistance to stopping driving is common because driving is often closely linked to independence and self-sufficiency. Families should approach the conversation with empathy and understanding. They can start by discussing specific concerns and observations and suggesting a professional driving evaluation for an objective assessment. If resistance continues, involving a healthcare professional such as a doctor or an occupational therapist may help provide a neutral perspective and reinforce the importance of safety.
3. Are there resources available for older adults to continue driving safely?
Yes, several resources are available to help older adults drive safely. Adaptive driving evaluations through hospital rehabilitation programs or specialized driving schools can assess both physical and cognitive abilities and recommend adaptive equipment or modifications. Additionally, driver refresher courses specifically designed for older adults can help them brush up on their skills and learn new techniques to compensate for any deficits.
4. What are some alternatives to driving for older adults who can no longer drive safely?
There are many alternatives to driving that can help maintain an older adult’s independence. Options include public transit, rideshare services like Uber or Lyft, community shuttles, volunteer driver programs, and family or friends providing rides. Many communities also offer transportation services specifically designed for seniors, such as paratransit services or senior ride programs.
5. How can families support an older adult who has stopped driving to prevent isolation and depression?
Stopping driving can lead to feelings of isolation and depression due to reduced social interaction and freedom. Families can support their loved ones by encouraging participation in social activities that do not require driving, such as community events, clubs, or senior centers. Offering regular rides to social events, checking in frequently, and ensuring they remain engaged with their community are also helpful strategies.
6. How often should older adults be re-evaluated for their driving abilities?
There is no one-size-fits-all answer, as re-evaluation frequency depends on the individual’s health condition. Generally, if an older adult shows any signs of cognitive decline, physical impairment, or behavioral changes that might affect their driving, they should be re-evaluated by a healthcare professional or through a professional driving assessment. Otherwise, periodic assessments every year or two might be sufficient, especially if there are underlying health concerns.
By addressing these common questions, families can be better prepared to navigate the challenging, yet important, conversations about driving safety with their older loved ones.