Imagine This:
You’ve been feeling a bit forgetful lately, struggling to recall names and dates that used to come easily to you. Concerned, you visit your doctor, who suggests an MRI of the brain to check things out. A week later, you sit in your doctor’s office as they explain the results: "Your MRI shows moderate subcortical microvascular ischemic disease." You nod, but inside, you’re worried. What does this mean? Is it serious? Should you be scared?
This scenario is common, and many patients leave with more questions than answers. Let's break down what these findings mean and why they don't necessarily spell doom.
What is White Matter Disease?
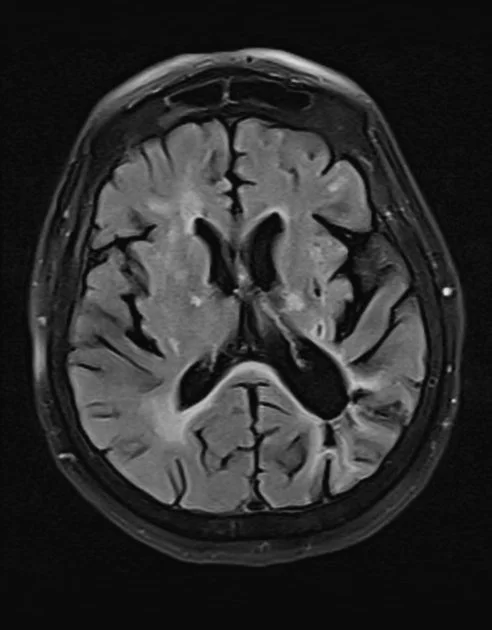
An MRI of the brain showing white matter hyperintensities.
White matter disease refers to changes in the brain's white matter, the part of the brain responsible for communication between different brain regions and between the brain and spinal cord. These changes are often detected through MRI scans and can appear as small, bright spots on the images. These spots indicate areas where the white matter has been damaged or has degenerated.
Causes and Risk Factors
White matter disease is primarily associated with aging but can also result from conditions that affect the small blood vessels in the brain, such as:
Hypertension: High blood pressure can damage the small blood vessels in the brain, leading to reduced blood flow and white matter changes.
Diabetes: Poorly controlled blood sugar levels can also contribute to these changes.
Smoking: Smoking increases the risk of vascular disease, which can affect brain health.
High Cholesterol: Elevated cholesterol levels can lead to the buildup of plaques in blood vessels, reducing blood flow to the brain.
Do You Bruise Easily?
Think of it like this: as people get older, they often bruise more easily because their blood vessels become more fragile. This is similar to what happens in the brain. The small blood vessels supplying the brain can also weaken and become more prone to damage with age. Just as a minor bump might cause a noticeable bruise on the skin of an older person, minor issues in the blood vessels of the brain can show up as white matter changes on an MRI.
Is It Normal or Abnormal?
It's essential to understand that some degree of white matter change is a normal part of aging. Many older adults show these changes on MRI without any symptoms or with only mild cognitive impairments. However, extensive white matter disease can indicate a higher risk of more severe conditions, such as:
Lacunar Infarcts: Small strokes that occur in the deep parts of the brain due to the occlusion of small penetrating arteries.
Cognitive Decline: More extensive white matter changes have been linked to difficulties with executive functions, processing speed, and memory.
Will It Get Worse?
The progression of white matter disease can vary. For some individuals, these changes may remain stable for years without causing significant problems. For others, especially those with uncontrolled risk factors like hypertension or diabetes, the condition may worsen over time. Regular monitoring and managing these risk factors are crucial to slowing the progression.
Does It Mean I Will Get Dementia?
Not necessarily. While extensive white matter changes are associated with a higher risk of cognitive decline and dementia, many people with these changes do not develop dementia. The risk depends on several factors, including the extent of the changes, the presence of other conditions like Alzheimer's disease, and overall brain health. Early detection and management of risk factors play a significant role in maintaining cognitive function.
Symptoms and Clinical Significance
In many cases, white matter disease is asymptomatic and discovered incidentally during imaging for other reasons. When symptoms do occur, they can include:
Cognitive Impairment: Slower processing speed, memory problems, and difficulties with executive functions.
Gait Abnormalities: Difficulty walking or maintaining balance.
Mood Changes: Increased risk of depression and mood disorders.
Diagnosis and Monitoring
MRI is the most sensitive method for detecting white matter changes. Regular monitoring through follow-up imaging can help assess the progression of the disease and its impact on cognitive function. Additional assessments might include neuropsychological tests to evaluate cognitive abilities and identify any decline over time.
Management and Prevention
While there is no cure for white matter disease, managing risk factors can slow its progression and reduce the risk of associated complications:
Blood Pressure Control: Keeping blood pressure within a normal range can prevent further damage.
Blood Sugar Management: Proper diabetes management is crucial.
Healthy Lifestyle: Quitting smoking, eating a balanced diet, and regular exercise can improve overall vascular health.
Medication: In some cases, doctors might prescribe medications to manage symptoms or control risk factors, such as antihypertensives or statins.
Conclusion
White matter disease, as seen on MRI, can be a common finding, especially in older adults. While it may be part of the normal aging process, extensive changes can signal more significant health concerns. Understanding these findings can help alleviate fears and emphasize the importance of managing risk factors to maintain brain health.
If you have questions or concerns about your MRI results, discussing them with your healthcare provider can provide clarity and guide appropriate next steps.