Introduction
Have you ever wondered if your snoring is more than just an annoyance? Sure, your sleep-deprived partner may have nagged you about getting it checked out, but there are also real medical concerns that could be at play. Sleep apnea, a common yet serious sleep disorder, might be the culprit behind your daytime fatigue and cognitive difficulties. In this blog post, we'll explore what sleep apnea is, debunk some common myths, examine its impact on cognition, and discuss various treatment options.
What is Sleep Apnea?
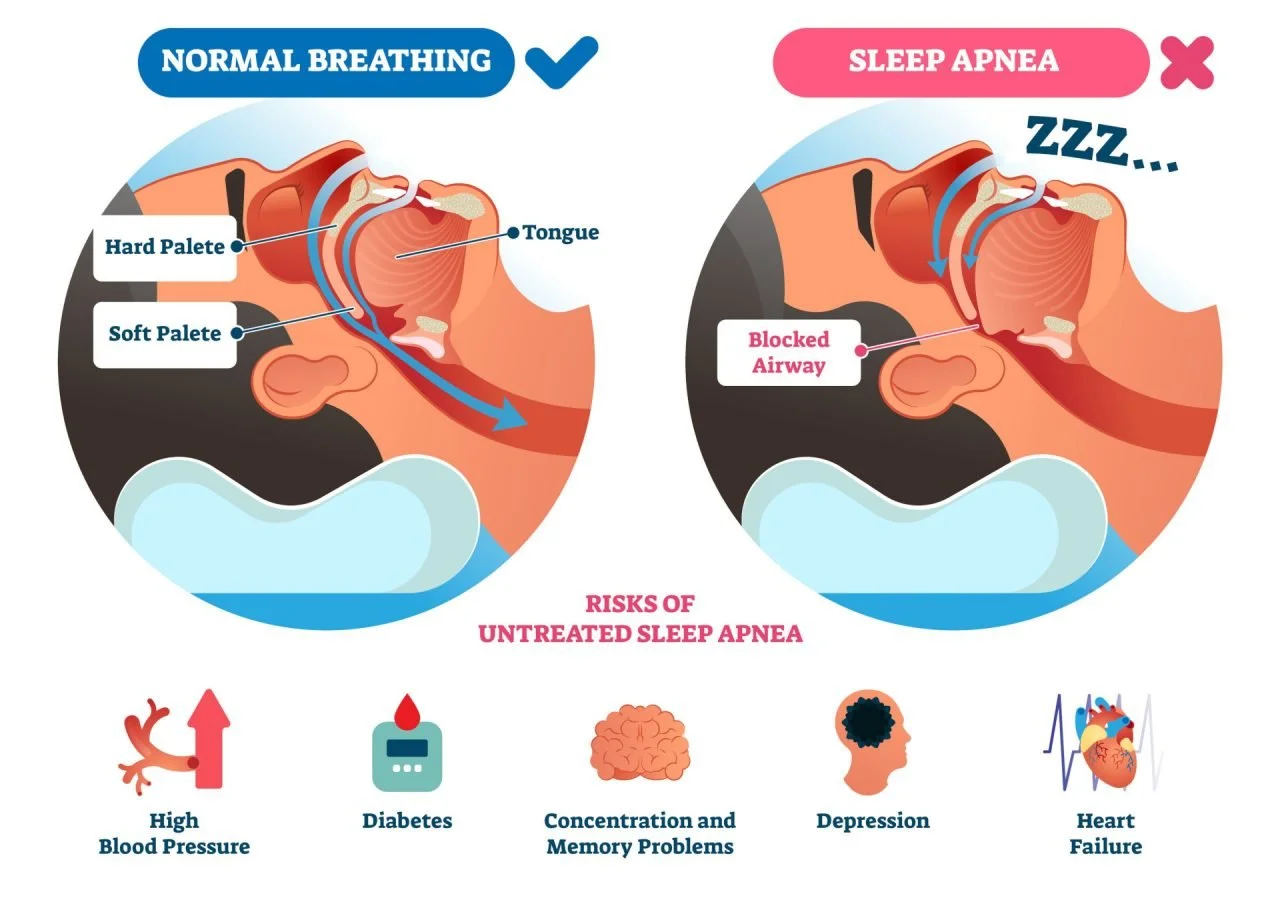
Sleep apnea is a disorder characterized by repeated interruptions in breathing during sleep. These interruptions, or apneas, can occur dozens or even hundreds of times per night, leading to poor sleep quality and various health issues. There are two main types of sleep apnea:
Obstructive Sleep Apnea (OSA): The more common form, caused by a blockage of the airway, usually when the soft tissue at the back of the throat collapses during sleep.
Central Sleep Apnea (CSA): Occurs when the brain fails to signal the muscles to breathe due to instability in the respiratory control center.
Common Misconceptions about Sleep Apnea
Myth 1: Snoring is harmless: While snoring itself can be benign, it can also be a sign of sleep apnea, which is not harmless. Snoring combined with choking or gasping sounds may indicate a serious problem.
Myth 2: Only older, overweight individuals get sleep apnea: Sleep apnea can affect people of all ages and body types, including children and individuals of normal weight.
Myth 3: Sleep apnea is just about sleep: The disorder has far-reaching effects beyond just poor sleep. It increases the risk of cardiovascular diseases, diabetes, and cognitive decline.
How Sleep Apnea Impacts Cognition
The repeated awakenings and reduced oxygen supply caused by sleep apnea lead to fragmented sleep and decreased blood flow to the brain. This can result in:
Memory Loss: Difficulty in forming new memories and recalling information.
Reduced Attention and Concentration: Trouble focusing on tasks and maintaining attention.
Impaired Executive Function: Challenges in planning, decision-making, and problem-solving.
One critical process affected by sleep apnea is memory consolidation. Memory consolidation occurs during sleep, particularly during deep sleep (slow-wave sleep) and REM sleep, when the brain processes and stores information gathered throughout the day. Sleep apnea disrupts these stages of sleep, leading to:
Interrupted Memory Consolidation: The constant waking prevents the brain from effectively transferring information from short-term to long-term memory.
Impaired Learning and Recall: The disruption of sleep cycles hinders the brain's ability to solidify learning and make new memories accessible when needed.
Research has shown a strong link between sleep apnea and cognitive impairments. For example, studies indicate that untreated sleep apnea can increase the risk of developing dementia.
Treatment Options for Sleep Apnea
Effective treatment of sleep apnea can improve sleep quality and mitigate cognitive impairments. Here are some common treatment approaches:
Continuous Positive Airway Pressure (CPAP) machine.
Continuous Positive Airway Pressure (CPAP): Delivers a constant stream of air through a mask to keep the airway open during sleep.
Bi-level Positive Airway Pressure (BiPAP): Provides two levels of pressure—higher when you inhale and lower when you exhale.
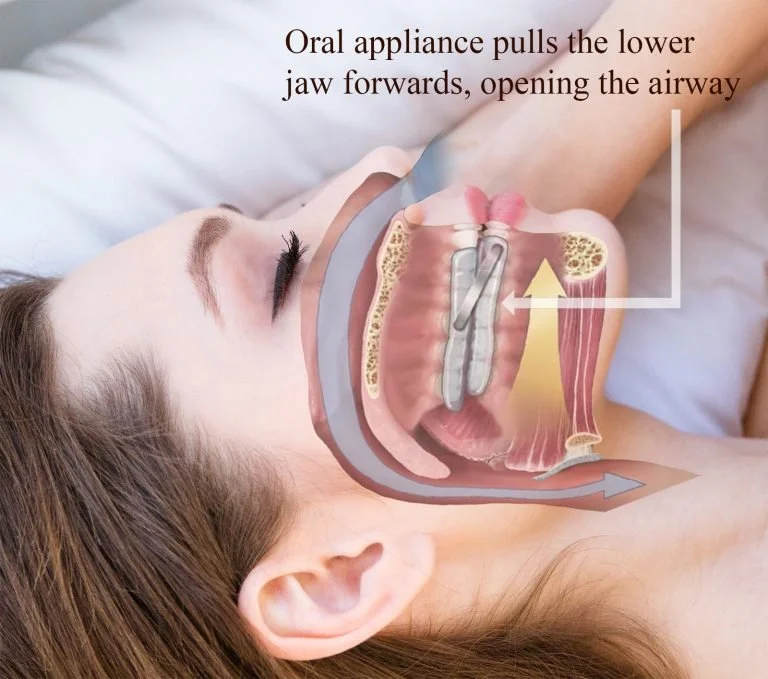
Oral Appliances:
Mandibular Advancement Devices (MADs): Fit over the upper and lower teeth and advance the lower jaw slightly forward.
Tongue Retaining Devices (TRDs): Hold the tongue in a forward position to prevent it from obstructing the airway.
Surgical Options:
Uvulopalatopharyngoplasty (UPPP): Removes tissue from the throat to widen the airway.
Genioglossus Advancement (GA): Repositions the muscle that attaches the tongue to the lower jaw.
Maxillomandibular Advancement (MMA): Moves the upper and lower jaw forward to enlarge the airway.
Radiofrequency Ablation (RFA): Uses energy to shrink tissues in the airway.
Inspire Therapy: A surgically implanted device that stimulates airway muscles.
Positional Therapy: Uses devices to prevent sleeping on the back.
Lifestyle Changes:
Weight Loss: Can significantly improve or resolve sleep apnea.
Smoking Cessation: Reduces inflammation and fluid retention in the airway.
Alcohol Reduction: Helps keep the airway open.
Emerging and Alternative Treatments:
Expiratory Positive Airway Pressure (EPAP): Single-use devices placed over the nostrils.
Myofunctional Therapy: Exercises to strengthen the muscles around the airway.
Hypoglossal Nerve Stimulation: Electrical stimulation of the nerve controlling tongue movement.
One type of oral appliance for sleep apnea
FAQs
Which treatments are most effective for sleep apnea? CPAP is generally considered the most effective treatment for moderate to severe obstructive sleep apnea. However, BiPAP, oral appliances like MADs and TRDs, and surgical options can also be effective depending on the severity of the condition and patient preferences.
What can I do if CPAP is hard to tolerate? If CPAP is difficult to tolerate, you can try adjusting the mask fit, using a humidifier, or trying a different type of mask. Additionally, you might consider alternative treatments such as BiPAP, oral appliances, or positional therapy. Consulting with a sleep specialist can help you find the most comfortable and effective solution.
Is the memory loss from sleep apnea permanent? Memory loss from sleep apnea is often reversible with effective treatment. Once the sleep apnea is managed and normal sleep patterns are restored, many individuals experience improvements in memory and cognitive function. However, prolonged untreated sleep apnea can lead to more lasting cognitive deficits.
How is sleep apnea diagnosed? Sleep apnea is typically diagnosed through a sleep study, also known as polysomnography. This can be done in a sleep lab or at home with a portable monitoring device. The study records various body functions during sleep, such as brain activity, eye movements, heart rate, breathing patterns, oxygen levels, and muscle activity.
What are the long-term health risks associated with untreated sleep apnea? Untreated sleep apnea can lead to a range of serious health issues, including high blood pressure, heart disease, stroke, diabetes, and an increased risk of accidents due to daytime sleepiness. It can also contribute to mental health problems such as depression and anxiety.
Is sleep apnea hereditary? There is evidence to suggest that sleep apnea can run in families, indicating a genetic component. Factors such as inherited physical traits (e.g., a narrow airway) and family history of sleep disorders can increase the risk.
Can sleep apnea be cured? While there is no outright cure for sleep apnea, many effective treatments can significantly reduce symptoms and improve quality of life. In some cases, weight loss or surgical interventions can lead to a resolution of symptoms.
Can sleep apnea affect mental health? Yes, sleep apnea can negatively impact mental health. Chronic sleep deprivation and oxygen deprivation can contribute to mood disorders, such as depression and anxiety. Effective treatment of sleep apnea often leads to improvements in mental well-being.
Conclusion
Snoring might seem like a minor inconvenience, but it could be a sign of sleep apnea, a disorder with serious cognitive implications. If you or a loved one experiences symptoms of sleep apnea, it's crucial to seek medical evaluation and explore appropriate treatment options. Prioritizing your sleep health can lead to significant improvements in your overall well-being and cognitive function. Plus, your partner will thank you for the quiet nights!
Call to Action
If you think that you or a loved one is suffering from memory loss due to sleep apnea, reach out to us about an assessment!